Acute Thrombotic Microangiopathy
- Thrombotic microangiopathy (TMA) is characterized by thrombocytopenia and microangiopathic hemolytic anemia (MAHA), results from acute and/or chronic endothelial cell injury, and often manifests with kidney dysfunction.
- TMA can be observed in a wide spectrum of clinical scenarios.
- When a clinical and/or pathologic diagnosis of TMA is established, it is essential to exclude TTP as a potential cause. TTP results from an inherited or acquired deficiency of ADAMTS13 activity, a plasma protein that cleaves the ultralarge multimers of von Willebrand factor (vWF). Most cases are due to acquired autoantibodies to ADAMTS13, which may arise in the setting of autoimmune disorders, pregnancy, drug reaction, malignancy, and infection.
- After a diagnosis of TTP has been excluded, classic (or typical) HUS (caused by Shiga toxin-producing bacteria including Escherichia coli O157:H7 / 0104:H4 or Shigella dysenteriae), anti-phospholipid antibody syndrome (APS), malignant hypertension, systemic sclerosis (scleroderma renal crisis), atypical HUS (aHUS), disseminated intravascular coagulation (DIC), pharmacologic agents, etc. can be considered and appropriately worked-up.
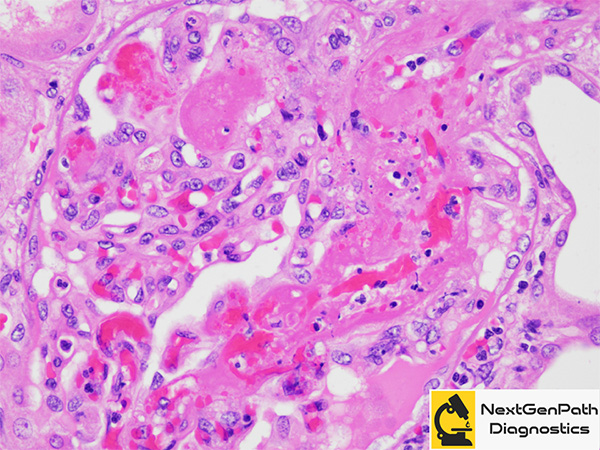
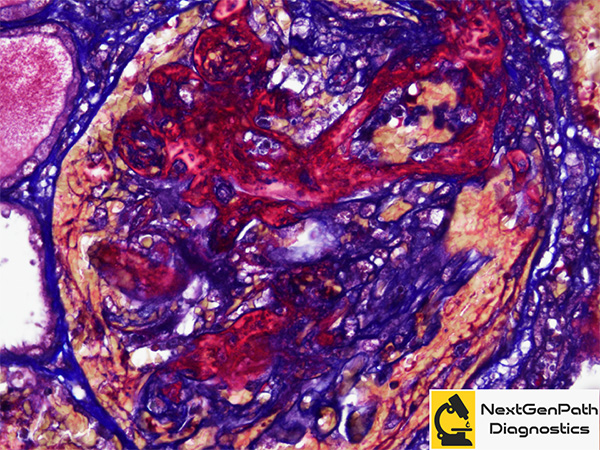
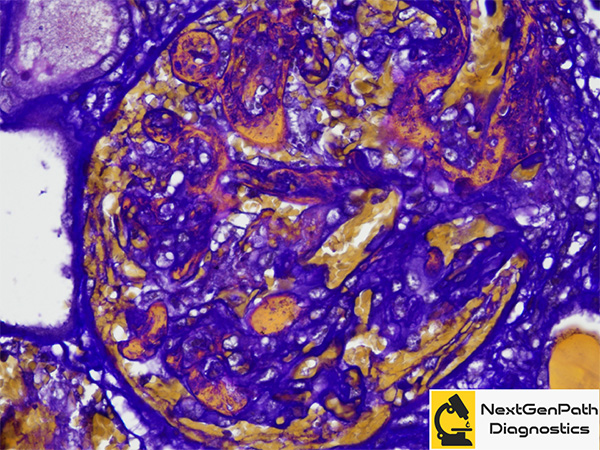
- Renal biopsy: Microscopically, acute TMA is characterized by occlusion and distention of small vessels (glomeruli and/or arterioles) by thrombi with frequent presence of fragmented red blood cells (schistocytes), WBC nuclear debris and associated endothelial cell swelling. Glomeruli can frequently demonstrate ischemic changes and even the variants of focal segmental glomerulosclerosis, including the collapsing variant.
- Diagnosis and Management: Establishing the cause of a TMA is usually possible after a complete evaluation. The decision-making is time-critical: the initial priority should be the consideration of TTP, because urgent management is imperative given the high mortality if untreated, and therefore in adults, plasma exchange (PE) should be instituted (after obtaining a sample for ADAMTS13 activity testing) on the presumption that it is TTP unless other evidence is available that strongly suggests an alternative cause. If the ADAMTS13 result excludes TTP, then complement-mediated aHUS is presumed and treatment with eculizumab is recommended, pending the complete evaluation. In children, in whom PE may not be appropriate and is high risk, treatment with eculizumab has been recommended by Kidney Disease: Improving Global Outcomes before the availability of the ADAMTS13 result, with the caveat that clinical deterioration on eculizumab should necessitate immediate plasma therapy.
References
- Gallan AJ, Chang A. A new paradigm for renal thrombotic microangiopathy. Semin Diagn Pathol. 2020;37:121-126.
- Brocklebank V, Wood KM, Kavanagh D. Thrombotic microangiopathy and the kidney. Clin J Am Soc Nephrol. 2018;13:300-317.